As far as break-ups go, dealing with a clingy infection can be nothing short of a nightmare! Whether it’s a slow-healing skin infection that always re-emerges; persistent and painful sinus infections; or just having the worst luck attracting every germ going around – it’s time to audit immune function. Why? Because it’s possibly not about the infection itself – it’s about the body’s ability to sustain an effective immune response. Let me explain…
Immune performance is a report card of many habits
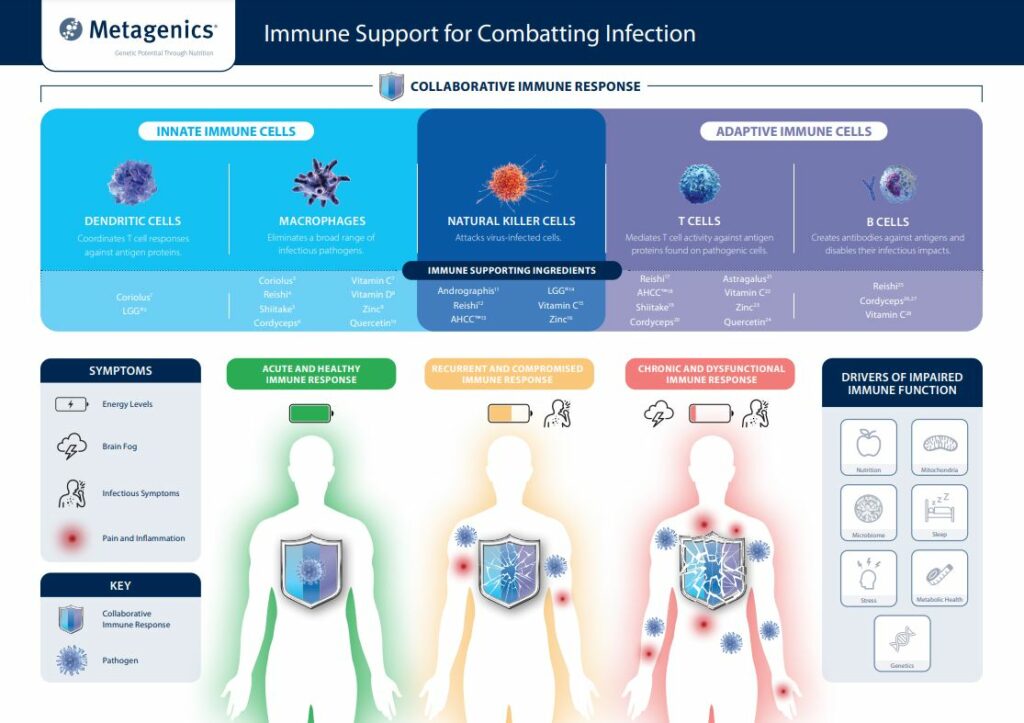
When infections become persistent, it’s time to assess daily habits and general health. This can help determine ‘areas of improvement’ to restore peak immune performance. Beyond basic personal hygiene, our defensive ability against infection is most effective when we prioritise healthy nutritional choices, get enough restful sleep and maintain beneficial levels of protective gut bacteria. These factors are key for supporting strong immune barriers (e.g., skin and nasal membranes) that trap and destroy microbes before they can flourish. Additionally, these habits can influence the body’s ability to form a robust team of innate and adaptive immune cells that target invading pathogens.
Outside of these aspects, persistent tissue inflammation may also contribute to prolonged infection. For example, intense exercise that exceeds physical activity guidelines, chronic work-related, personal or mental stress and toxin exposure (e.g., cigarettes and alcohol) can all compromise immune barriers. Consequently, budding infections can gain momentum – making it difficult for the immune system to control their spread. In addition, other inflammatory health issues (such as being overweight) can also diminish immune function, especially as we age. As it goes, maintaining a high-performing immune response depends on the foundations we build!

Antibiotics and immune health: the problem with throwing the good bugs out with the bad
Research shows that the microbiome has evolved with us to help fight infection. In fact, the number of cells within our gut microbiota outnumbers our body cells 4:1 – so it’s important to consider the bugs that make up 80% of the body. When it comes to infections, antibiotic treatments for common pathogens (such as Staphylococcus aureus and Escherichia coli ) have been shown to reduce levels of essential immune-enhancing species.1 This in turn can increase susceptibility to infections – especially against microbes that naturally coexist on barrier surfaces, which can flourish when host immunity is impaired.
Specifically, antibiotic use is linked to reduced levels of the immune-supporting bacterial metabolite, butyrate. In action, butyrate controls pathogen growth through several mechanisms, which help to repair barrier damage caused by infection. As such, maintaining a healthy microbiome abundant with butyrate-producing gut microbiota can prevent infections from hanging around – especially in patients with a history of antibiotic use.
To learn about how to restore a healthy gut microbiome, check out this blog for more info!
Other ways to speed up the healing process, naturally
Aside from healthy habits and the microbiome, natural medicines outlined in the infographic below can lower infection risk, particularly against recurrent infections. For instance, medicinal mushrooms cordyceps, coriolus and reishi have been found elevate innate and adaptive immune cells over 8 weeks in human clinical trials.2,3,4 In the same vein, zinc intake promotes healthy mucosal barriers, in addition to boosting the synthesis of immune cells.5,6 Importantly, data indicates that over a quarter of men and 10% of women in Australia are likely to be zinc deficient, highlighting the benefits of taking zinc to help conquer infection.
Break it off with infections and move onto the next chapter
Life is too short to be fighting with infections that hold us back. For better immune health, individuals can audit habits, support the gut microbiome and stimulate natural immunity to shut down infections before they become an ongoing battle. By taking your advice, patients can move forward with a strong and sturdy immune response!
References
1 Zhang S, Chen DC. Facing a new challenge: the adverse effects of antibiotics on gut microbiota and host immunity. Chin Med J (Engl). 2019 May 20;132(10):1135-1138. doi: 10.1097/CM9.0000000000000245
2 Jung SJ, Jung ES, Choi EK, Sin HS, Ha KC, Chae SW. Immunomodulatory effects of a mycelium extract of Cordyceps (Paecilomyces hepiali; CBG-CS-2): a randomized and double-blind clinical trial. BMC Complement Altern Med. 2019;19(1):77. doi: 10.1186/s12906-019-2483-y
3 Munroe JE. Chronic fatigue immune dysfunction syndrome. J Integrative Medicine. 2004;8:101-8.
4 Henao SLD, Urrego SA, Cano AM, Higuita EA. Randomized clinical trial for the evaluation of immune modulation by yogurt enriched with β-glucans from lingzhi or reishi medicinal mushroom, Ganoderma lucidum (agaricomycetes), in children from Medellin, Colombia. Int J Med Mushrooms. 2018;20(8):705-716. doi: 10.1615/IntJMedMushrooms.2018026986
5 Gombart AF, Pierre A, Maggini S. A review of micronutrients and the immune system: working in harmony to reduce the risk of infection. Nutrients. 2020;12(1):236. doi: 10.3390/nu12010236
6 Heller RA, Sun Q, Hackler J, et al. Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker. Redox Biol. 2021;38:101764. doi: 10.1016/j.redox.2020.101764









Leave a Comment