Feminine flora is a profoundly protective influence when it comes to reproductive health. In fact, evidence shows that an abundance of beneficial bacteria can support healthy conception,1 protect against bacterial vaginosis,2 vulvovaginal candidiasis (i.e., thrush),2 sexually acquired infections,3 and even cancers of the reproductive tract.4 To support vaginal health, we’ve shared three steps to help Practitioners nurture the vaginal microbiome.
Step 1: Learn about the importance of lactobacilli
A healthy vagina has high levels of lactobacilli, which helps maintain a balance of beneficial microbial species within intimate areas.1 These protective bacteria produce hydrogen peroxide and lactic acid, which keep the vaginal pH between 3.8 to 4.5. In addition, lactobacilli also produce antimicrobial compounds known as bacteriocins to fight off infection. Collectively, these bacterial by-products help prevent the growth of infectious bacteria before they can cause harm. 5,6 It’s amazing how the natural balance of vaginal flora can provide such protection! Considering this, reduced levels of lactobacilli can cause various problems, including urinary tract infections (UTIs), vaginal dysbiosis and thrush.2,8 Therefore, it’s crucial to limit disruptions to the vaginal microbiome to maintain a healthy balance.
Step 2: Consider disruptive factors that impact vaginal flora
The vaginal microbiome can be affected by several factors. Most commonly, individuals can experience disruptions in response to antibiotic use,9 fluctuating oestrogen levels (e.g., hormonal contraceptives,3 pregnancy,5 menopause10), uncontrolled diabetes11 and exposure factors including sexual activity and products designed for vaginal use.12,13
These elements influence the vaginal microbiome in various ways. For instance, while antibiotics eliminate harmful bacteria, they can also eradicate beneficial lactobacilli.9 This can lead to an increased risk of infections due to changes in the protective pH of the vagina.
Further, increases in oestrogen levels (e.g., due to some hormonal contraceptives3 and in pregnancy5) can increase the concentration of natural sugars (i.e., glycogen) in vaginal secretions, which can boost the growth of organisms. During menopause, less oestrogen comes with diminished glycogen levels, which can disturb healthy pH and contribute to the onset of vaginal infections.10
In uncontrolled diabetes,11 high blood sugar levels can also fuel the growth of microbes. In some individuals, increased sugar availability can also promote Candida albicans proliferationand ignite angry thrush symptoms – especially if lactobacilli levels are low.
Lastly, exposure factors can alsosway the balance of vaginal flora. For example, male ejaculate can neutralise vaginal pH for several hours,12 while the use of intimate products (e.g., lubricants, sex toys and hygiene products) can also disrupt the vaginal microbiome.13 While these factors are temporary in nature, they can still cause flora disruption.
Step 3: Boost vaginal lactobacilli to restore balance
To support vaginal lactobacilli levels, Probiotics Lactobacillus rhamnosus (GR-1™) and Lactobacillus reuteri (RC-14™) with liquorice for women’s urogenital health have been demonstrated to restore vaginal lactobacilli following oral intake.14-19 Combined with deglycyrrhizinated liquorice root (GutGard® liquorice), these ingredients can help soothe mucosal inflammation20 and aid in the management of UTIs, bacterial vaginosis and vulvovaginal thrush (Figure 1).21-23 Paired with a holistic approach, the triple action therapy of GR-1™ and RC-14™ combined with GutGard® liquorice can help restore healthy feminine flora.
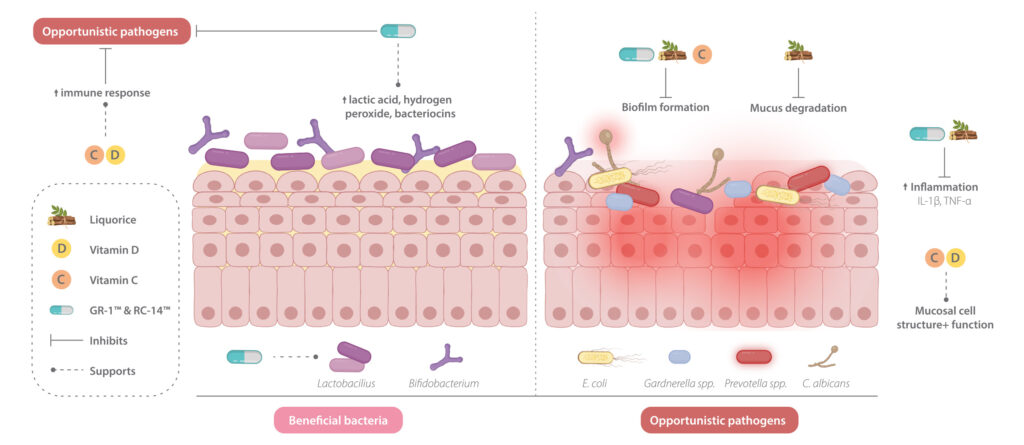
Figure 1: Benefits of natural ingredients to support vaginal health.
Nurture the lady microbiome
To maintain healthy vaginal flora, clinicians can prescribe Probiotics Lactobacillus rhamnosus (GR-1™) and Lactobacillus reuteri (RC-14™) with liquorice for women’s urogenital health to help cultivate better health outcomes in women experiencing vaginal dybiosis, thrush and UTIs.
If you’d like to read more on vaginal dysbiosis, we are a huge fan of this three part series on bacterial vaginosis that goes into more detail on this fascinating topic!
References
1. Vitale SG, Ferrari F, Ciebiera M, et al. The role of genital tract microbiome in fertility: a systematic review. Int J Mol Sci. 2021;23(1):180. doi:10.3390/ijms23010180
2. Zangl I, Pap IJ, Aspöck C, Schüller C. The role of Lactobacillus species in the control of Candida via biotrophic interactions. Microb Cell. 2019;7(1):1-14. doi:10.15698/mic2020.01.702
3. Cohen, K, Powderly, W, Opal, S, Calandra, T, Clumeck, N, Farrar, J, et al. Infectious Diseases. 4th edn. Brighton (UK):Elsevier; 2017.
4. Fan Q, Wu Y, Li M, et al. Lactobacillus spp. create a protective micro-ecological environment through regulating the core fucosylation of vaginal epithelial cells against cervical cancer. Cell Death Dis. 2021;12(12):1094. doi:10.1038/s41419-021-04388-y
5. Korenek P, Britt R, Hawkins C. Differentiation of the vaginoses-bacterial vaginosis, lactobacillosis, and cytolytic vaginosis. Int J Adv Nurs Pract. 2003;6(1):1-10.
6. Donders GG, Bellen G, Grinceviciene S, Ruban K, Vieira-Baptista P. Aerobic vaginitis: no longer a stranger. Res Microbiol. 2017 Nov – Dec;168(9-10):845-858. doi: 10.1016/j.resmic.2017.04.004.
7. Harmanli O, GY C, Nyirjesy P, Chatwani A, JP G. Urinary tract infections in women with bacterial vaginosis. Obstetrics Gynecol. 2000;95(5):710-712. doi:10.1097/00006250-200005000-00015
9. Clinical Key. Elsevier; 2020. Bacterial vaginosis. Updated April 23, 2020. Accessed April 29, 2020. https://www.clinicalkey.com.au
10. Kalia N, Singh J, Kaur M. Microbiota in vaginal health and pathogenesis of recurrent vulvovaginal infections: a critical review. Ann Clin Microbiol Antimicrob. 2020;19(1):5. doi:10.1186/s12941-020-0347-4
11. Zhang X, Liao Q, Wang F, Li D. Association of gestational diabetes mellitus and abnormal vaginal flora with adverse pregnancy outcomes. Medicine (Baltimore). 2018 Aug;97(34):e11891. doi: 10.1097/MD.0000000000011891.
12. Leppäluoto PA. Bacterial vaginosis: what is physiological in vaginal bacteriology? An update and opinion. Acta Obstet Gynecol Scandi. 2011 Dec;90(12):1302-6. doi:10.1111/j.1600-0412.2011.01279.x
13. Marrazzo JM, Thomas KK, Agnew K, Ringwood K. Prevalence and risks for bacterial vaginosis in women who have sex with women. STD. 2010 May;37(5):335-339.
14.Reid G, Charbonneau D, Erb J, et al. Oral use of Lactobacillus rhamnosus GR‐1 and L. fermentum RC‐14 significantly alters vaginal flora: randomized, placebo‐controlled trial in 64 healthy women. Fems Immunol Medical Microbiol. 2003;35(2):131-134. doi:10.1016/s0928-8244(02)00465-0
15. Vujic G, Knez AJ, Stefanovic VD, Vrbanovic VK. Efficacy of orally applied probiotic capsules for bacterial vaginosis and other vaginal infections: a double-blind, randomized, placebo-controlled study. Eur J Obstet Gyn R B. 2013;168(1):75-79. doi:10.1016/j.ejogrb.2012.12.031
16. Anukam K, Osazuwa E, Ahonkhai I, et al. Augmentation of antimicrobial metronidazole therapy of bacterial vaginosis with oral probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14: randomized, double-blind, placebo controlled trial. Microbes Infect. 2006;8(6):1450-1454. doi:10.1016/j.micinf.2006.01.003
17. Homayouni A, Bastani P, Ziyadi S, et al. Effects of probiotics on the recurrence of bacterial vaginosis. J Low Genit Tract Di. 2014;18(1):79-86. doi:10.1097/lgt.0b013e31829156ec
18. Reid G, Bruce AW. Urogenital infections in women: can probiotics help? Postgrad Med J. 2003;79(934):428. doi:10.1136/pmj.79.934.428
19. Younes JA, Lievens E, Hummelen R, Westen R van der, Reid G, Petrova MI. Women and their microbes: the unexpected friendship. Trends Microbiol. 2018;26(1):16-32. doi:10.1016/j.tim.2017.07.008
20. Mukherjee M, Bhaskaran N, Srinath R, et al. Anti-ulcer and antioxidant activity of GutGard. Indian J Exp Biol. 2010;48(3):269-274.
21.Jeavons HS. Prevention and treatment of vulvovaginal candidiasis using exogenous lactobacillus. J Obstetric Gynecol Neonatal Nurs. 2003;32(3):287-296. doi:10.1177/0884217503253439
22. Hickey RJ, Zhou X, Pierson JD, Ravel J, Forney LJ. Understanding vaginal microbiome complexity from an ecological perspective. Transl Res. 2012;160(4):267-282. doi:10.1016/j.trsl.2012.02.008
23. Gil NF, Martinez RCR, Gomes BC, Nomizo A, Martinis ECPD. Vaginal lactobacilli as potential probiotics against Candida SPP. Braz J Microbiol. 2010;41(1):6-14. doi:10.1590/s1517-8382201000010000









Leave a Comment