Ever since scientists fattened germ-free mice with ‘obese’ human gut microbes, [i],[ii] the role of the gut microbiome in weight regulation has been undoubted. However, human trials attempting to correct obesity with faecal microbial transplants (FMT) from healthy lean donors have thus far failed to support meaningful weight loss, despite beneficially improving the diversity of the gut microbiome,[iii] now known to be a key player in optimal health…and weight.
The human gut typically hosts around 37 trillion microbes, yet the genetic fingerprint of each person’s gut is unique. Despite this high level of individuality, a core set of bacterial species are present in most healthy individuals. Depletion or disturbance of this core bacterial population can shift the relationship within our gut from healthy symbiosis to dysbiosis (the term used to describe an unhealthy gut ecology), leading to a defensive inflammatory response. This constant low-grade inflammation triggers instability in the barrier lining the gut, sometimes called ‘leaky gut’, which can create gradual yet profound systemic effects linked to metabolic, vascular, neurological and immune diseases.[iv] Interestingly, it has been noted that obese patients tend to host lower microbial diversity, which may compromise important bacterial functions.[v] Why is this important?
Because the gut microbiome is a dynamic ecology which communicates far beyond the bowels to influence body composition, appetite and satiety.
An Unhappy Gut = An Unhappy Mind
Your gut microbes can be vulnerable to the stresses placed upon them, which includes the foods you choose to eat; with refined and processed ‘hyperpalatable’ foods (i.e. those made up of carbohydrates combined with fats and salt) easily disrupting the gut ecology. Inflammation created by this dysbiotic state can light a fire in the brain (termed ‘neuroinflammation’), which is linked to multiple mood disorders.[i] (You can read about the gut-mind connection here). In fact, it has been observed that psychological problems are experienced by up to 90% of obese patients, compared to 60% of normal weight individuals.[ii] A vicious cycle can occur as the same dietary and lifestyle pressures known to induce dysbiosis, also promote obesity,[iii] that is, high caloric intakes and a sedentary lifestyle. And these same factors are also linked to depression, anxiety and a heightened sensitivity to stress.[iv] Stress related ‘binge’ eating of excessive calories then triggers gut inflammation; a situation that can numb satiety signalling, leading to increased hunger,[v] and so it goes on. One of the big confounders here is this behaviour overrides the metabolic body weight set-point, pushing it ever higher, resulting in weight gain that becomes very hard to shift again. (Read more about the body weight set-point here).
Probiotics can Halt a Rising Body Weight Set-Point
Although FMT trials have failed to produce clear weight loss results, probiotics are instead offering hope. In a study carried out with mice, researchers found the probiotic Bifidobacterium animalis ssp lactis B-420™ helped offset the effects of eating a high fat diet, reducing weight gain. These mice also showed a reduction in toxins generated in the gut that can cross the gut barrier when it is ‘leaky’ creating systemic inflammation.[i] This is of interest as this type of metabolic inflammation is a driving force in developing metabolic syndrome and type 2 diabetes.[ii]
More importantly, a six month human trial in men confirmed these findings. The men received either 10 billion CFU[1]/day of Bifidobacterium animalis ssp lactis B-420™ or a placebo, with no particular dietary or lifestyle instruction offered, to find out what effect taking this probiotic had. Over the months, those taking a placebo continued on their path of gradually gaining weight, fat mass and waist size; however, the B-420™ probiotic group largely maintained their weight and fat mass, and actually reduced their waist size (see Figure 1). [iii]
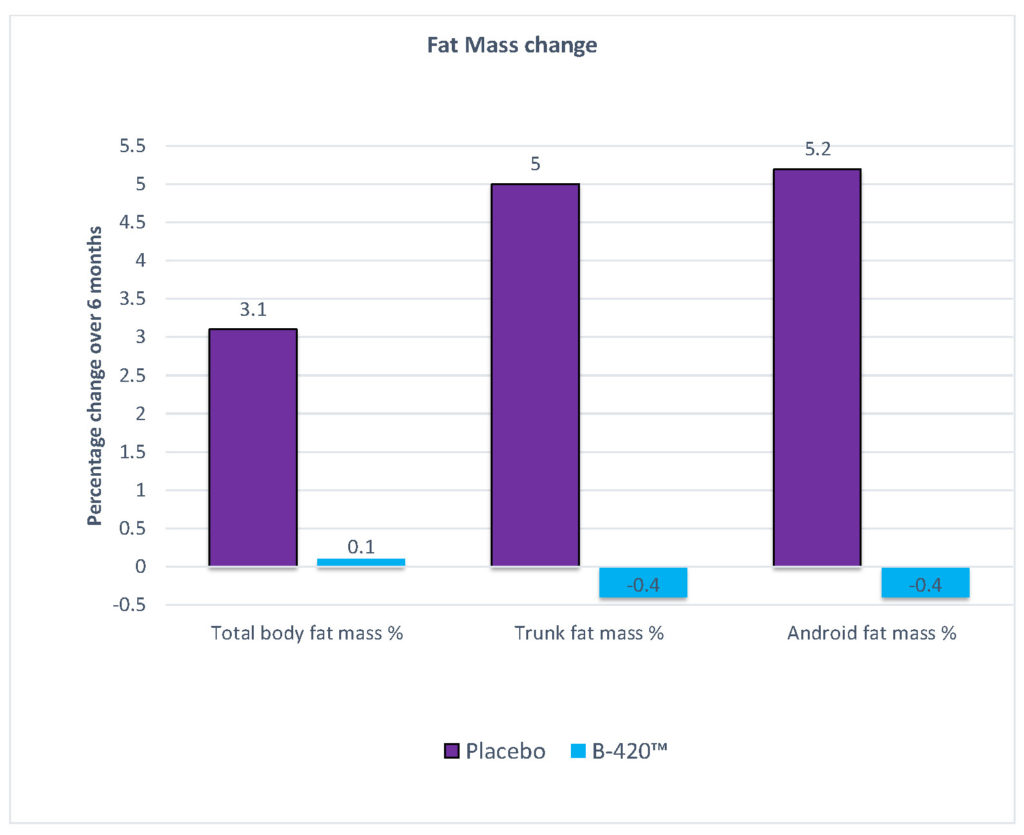
Figure 1. Fat mass change over six months probiotic supplementation with Bifidobacterium animalis ssp lactis B-420™ compared to placebo.
The fact that the B-420™ probiotic group unconsciously reduced their daily calories was arguably the most important finding of this study. That is, without even realising, they were consuming 320 fewer calories a day, and this was enough to halt ongoing weight gain. Meanwhile, the placebo group continued eating their previous calories and gradually gained, on average, 3 kg over six months.[i] These findings point to the specific effects of probiotic B-420™ to help normalise a healthy appetite and prevent insidious weight gain.
Obesity is strongly associated with increasing risks to cardiovascular disease, metabolic syndrome and/or type 2 diabetes,[ii] and these diseases have all been linked to dysbiosis.[iii] Similar to the B-420™ trial, the probiotic strain Bifidobacterium animalis ssp lactis HN019™ has been clinically trialled, but this time in metabolic syndrome patients. Over 45 days, patients received either 20 billion CFU/day of HN019™ or a placebo. Beyond the benefits of mildly reducing body mass index (BMI), the HN019™ group also exhibited reduced inflammation and improved lipid profiles including total cholesterol, and low-density lipoprotein (LDL), compared to no change in the placebo group.[iv]
Combining these two probiotic strains may help those whose dysbiosis is contributing to the complex issue of an unrelenting appetite in a setting of cardiovascular and metabolic risk.
Gut Microbiomes Love Lifestyle Medicine!
More good news is that our microbiome responds positively to wholefoods, regular sleep and physical activity, all of which supports healthy body weight regulation. For instance, a plant-rich diet delivers prebiotic fibres. Whilst not food for us, these non-soluble fibres stimulate bacterial diversity, resilience and healthy symbiosis in the colon.[v] Prebiotic fibres also contribute to a healthy weight by enhancing satiety sensitivity.[vi]
Research demonstrates better weight loss and metabolic outcomes in type 2 diabetics when consuming diverse carbohydrates and fibres in the diet.[vii]
Like us, our microbes also need rest and routine! Gut organisms exhibit daily rhythms influenced by feeding and produce measureable differences throughout the day. For instance, microbes engage in digestion, metabolism and environmental sensing during feeding, and between meals they repair, regenerate and detoxify.
Microbial molecular clocks are so sensitive to our feeding and sleeping rhythms that even common jet-lag can induce dysbiosis sufficiently enough to affect glucose intolerance and cause weight gain.[viii]
This points to the importance of regular sleep and eating patterns to maintain a healthy gut and waist line.

Let Your Microbiome Weigh In
Now that you know that your gut health can affect your weight, do you need to examine the role your diet and gut microbiome are playing in your situation?
With an imbalance in the gut microbiome known to interfere with weight regulation, the use of strain specific probiotic therapy, along with fewer calories, prebiotic rich wholefoods, sleep and exercise can help minimise food cravings during weight loss.
Furthermore, these strategies support gut microbiome resilience to help protect against obesity and its inflammatory comorbidities, including depression and osteoarthritis.
Whilst obviously a complex topic, you don’t need to navigate this alone. Talk to a natural healthcare Practitioner about the Shake It Practitioner Weight Management Program – a comprehensive solution that can be tailored to your personal needs. This program addresses all the elements that can help support a healthy gut microbiome, and lower your metabolic body weight set-point, so you can lose weight without feeling hungry and, most importantly, keep it off for the long-term. To start your journey toward better body composition today, click here to find a Practitioner near you.
[i] Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006 Dec 21;444(7122):1027-31. PubMed PMID: 17183312.
[ii] Ridaura VK, Faith JJ, Rey FE, Cheng J, Duncan AE, Kau AL, et al. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science. 2013 Sep 6;341(6150):1241214. doi: 10.1126/science.1241214.
[iii] van Nood E, Vrieze A, Nieuwdorp M, Fuentes S, Zoetendal EG, de Vos WM, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368(5):407-15. doi: 10.1056/NEJMoa1205037
[iv] Marotz CA, Zarrinpar A. Treating obesity and metabolic syndrome with fecal microbiota transplantation. Yale J Biol Med. 2016 Sep 30;89(3):383-388. eCollection 2016 Sep. Review. PubMed PMID: 27698622
[v] Sanmiguel C, Gupta A, Mayer EA. Gut Microbiome and obesity: A plausible explanation for obesity. Curr Obes Rep. 2015 Jun;4(2):250-61. doi: 10.1007/s13679-015-0152-0.
[i] Agustí A, García-Pardo MP, López-Almela I, Campillo I, Maes M, Romaní-Pérez M, et al. Interplay between the gut-brain axis, obesity and cognitive function. Front Neurosci. 2018 Mar 16;12:155. doi: 10.3389/fnins.2018.00155.
[ii] De Gara CJ, Karmali S. The anatomy of a weight recidivism and revision bariatric surgical clinic. Gastroenterol Res Pract. 2014;2014:721095. doi:10.1155/2014/721095.
[iii] Morris MC, Gilliam EA, Li L. Innate immune programing by endotoxin and its pathological consequences. Front Immunol. 2015 Jan 6;5:680. doi:10.3389/fimmu.2014.00680.
[iv] Agustí A, García-Pardo MP, López-Almela I, Campillo I, Maes M, Romaní-Pérez M, et al. Interplay between the gut-brain axis, obesity and cognitive function. Front Neurosci. 2018 Mar 16;12:155. doi: 10.3389/fnins.2018.00155.
[v] Valdearcos M, Douglass JD, Robblee MM, Dorfman MD, Stifler DR, Bennett ML, et al. Microglial inflammatory signaling orchestrates the hypothalamic immune response to dietary excess and mediates obesity susceptibility. Cell Metab. 2018 Jun 5;27(6):1356. doi: 10.1016/j.cmet.2018.04.019.
[1] Colony forming units
[i] Stenman LK, Waget A, Garret C, Klopp P, Burcelin R, Lahtinen S. Potential probiotic Bifidobacterium animalis ssp. lactis 420 prevents weight gain and glucose intolerance in diet-induced obese mice. Benef Microbes. 2014 Dec;5(4):437-45. doi: 10.3920/BM2014.0014. PubMed PMID: 25062610.
[ii] Cani PD, Osto M, Geurts L, Everard A. Involvement of gut microbiota in the development of low-grade inflammation and type 2 diabetes associated with obesity. Gut Microbes. 2012 Jul-Aug;3(4):279-88. PMID: 22572877.
[iii] Stenman LK, Lehtinen MJ, Meland N, Christensen JE, Yeung N, Saarinen MT, et al. Probiotic With or Without Fiber Controls Body Fat Mass, Associated With Serum Zonulin, in Overweight and Obese Adults-Randomized Controlled Trial. EBioMedicine. 2016 Nov;13:190-200. doi: 10.1016/j.ebiom.2016.10.036.
[i] Stenman LK, Lehtinen MJ, Meland N, Christensen JE, Yeung N, Saarinen MT, et al. Probiotic With or Without Fiber Controls Body Fat Mass, Associated With Serum Zonulin, in Overweight and Obese Adults-Randomized Controlled Trial. EBioMedicine. 2016 Nov;13:190-200. doi: 10.1016/j.ebiom.2016.10.036.
[ii] Australian Government. Australian Institute of Health and Welfare. Risk factors to health [Internet]. 2017 [updated 2017 Aug 7; cited 2017 Sept 21]. Available from: https://www.aihw.gov.au/reports/biomedical-risk-factors/risk-factors-to-health/contents/risk-factors-and-disease-burden
[iii] Zhao L, Zhang F, Ding X, Wu G, Lam YY, Wang X, et al. Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science. 2018 Mar 9;359(6380):1151-6.
[iv] Bernini LJ, Simão AN, Alfieri DF, Lozovoy MA, Mari NL, de Souza CH, et al. Beneficial effects of Bifidobacterium lactis on lipid profile and cytokines in patients with metabolic syndrome: A randomized trial. Effects of probiotics on metabolic syndrome. Nutrition. 2016 Jun;32(6):716-9. doi:10.1016/j.nut.2015.11.001.
[v] Gibson G.R., Roberfroid M.B. Dietary modulation of the human colonic microbiota: Introducing the concept of prebiotics. J. Nutr. 1995;125:1401–1412. PubMed PMID: 7782892.
[vi] Cani P.D., Delzenne N.M. Interplay between obesity and associated metabolic disorders: New insights into the gut microbiota. Curr. Opin. Pharmacol. 2009;9:737–743. doi: 10.1016/j.coph.2009.06.016.
[vii] Zhao L, Zhang F, Ding X, Wu G, Lam YY, Wang X, et al. Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science. 2018 Mar 9;359(6380):1151-6. doi: 10.1126/science.aao5774.
[viii] Thaiss CA, Zeevi D, Levy M, Zilberman-Schapira G, Suez J, Tengeler AC, et al. Transkingdom control of microbiota diurnal oscillations promotes metabolic homeostasis. Cell. 2014 Oct 23;159(3):514-29. doi: 10.1016/j.cell.2014.09.048.









Leave a Comment